BREAST CANCER
Let us help you stay informed
What is breast cancer
Breast cancer is a disease in which cells in the breast grow out of control. There are different kinds of breast cancer. The kind of breast cancer depends on which cells in the breast turn into cancer.
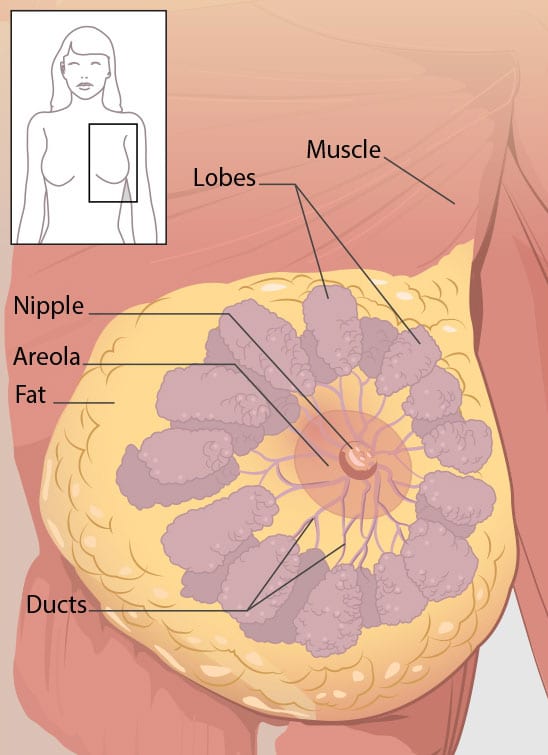
Breast cancer can begin in different parts of the breast. A breast is made up of three main parts: lobules, ducts, and connective tissue. The lobules are the glands that produce milk. The ducts are tubes that carry milk to the nipple. The connective tissue (which consists of fibrous and fatty tissue) surrounds and holds everything together. Most breast cancers begin in the ducts or lobules.
Breast cancer can spread outside the breast through blood vessels and lymph vessels. When breast cancer spreads to other parts of the body, it is said to have metastasized.
Kinds of Breast Cancer
The most common kinds of breast cancer are—
- Invasive ductal carcinoma. The cancer cells grow outside the ducts into other parts of the breast tissue. Invasive cancer cells can also spread, or metastasize, to other parts of the body.
- Invasive lobular carcinoma. Cancer cells spread from the lobules to the breast tissues that are close by. These invasive cancer cells can also spread to other parts of the body.
- Ductal carcinoma in situ(DCIS) is a breast disease that may lead to breast cancer. The cancer cells are only in the lining of the ducts, and have not spread to other tissues in the breast.
There are several other less common kinds of breast cancer, such as Paget’s disease, medullary, mucinous, malignant phyllodes tumor and inflammatory breast cancer.
Found a lump in your breast?
Finding a lump in your breast can be alarming. Although breast cancer is the most common type of cancer found in women, not all lumps are cancer. Often, a lump in your breast can be caused by a benign breast mass or a fluid-filled breast cyst.
Yet in some cases, a cancerous lump in your breast can be too small to feel or cause any noticeable changes in your breast. Sometimes patients don’t experience any signs or symptoms of breast cancer. These types of breast cancer can only be diagnosed by having regular yearly mammograms and other screening tests.
However, as a rule of thumb, if you feel a change in your breast – something different or new – you should reach out to breast surgeon such as Dr. Kolluri for evaluation.
Symptoms of breast cancer
Breast health and breast self-awareness
Knowing how your breasts feel and look is a critical aspect of breast health. There is no such thing as an idyllic breast. What may feel normal to you may not be normal for others.
Most women examining their breasts for the first time say that their breasts are lumpy. Medication, periods, having children, losing or gaining weight are some of the factors that affect the way your breasts look and feel. Also, your breasts often change in size, shape and texture as you age.
It is important for you to maintain routine breast-self awareness of what is normal for your breasts, and be aware of any changes in your breasts. Knowing the signs and symptoms of breast cancer will help your breast surgeon provide the best possible care to you.
Signs and symptoms of breast cancer
According to the American Cancer Society, any of the following unusual changes in the breast can be a symptom of breast cancer:
- a breast mass which is not painful
- swelling of all or part of the breast (even if no lump is felt)
- skin dimpling or nipple retraction (nipple turning inward)
- redness, scaliness, or thickening of the nipple or breast skin
- a nipple discharge other than breast milk, such as blood or clear fluid from a single duct opening
- a lump in the underarm
Breast cancer diagnosis
Breast cancer that is found early and has not spread is much easier to treat successfully. Since breast cancer tumors can be too small to show up as a lump or a visible change in your breast, the best way to find a tumor is to get regular screening mammograms.
Breast self-exam / breast self-awareness
Performing breast self awareness should be a part of everybody’s daily health care routine. It is critical to both visually inspect and self-palpate all areas of your breast, including your skin, breast tissue, nipple and underarm. This should be done throughout the month, so that you can get a sense of how your breast changes with your menstrual cycles, and what is normal for you. Your goal is to not only look for a lump in your breasts that you can feel, but also thoroughly examine your breasts for other more subtle changes in your breasts such as nipple changes or skin dimpling.
How often should a woman with average breast cancer risk get a screening?
Mammograms
A screening mammogram is a type of imaging that uses a very low dose digital X-ray to evaluate your breasts. Doctors use mammograms to find a cancer in your breast that is still in its very early stages – even before the clinical signs and symptoms of cancer appear – thereby giving you a better chance at a successful treatment and recovery. Mammograms catch 85 percent of all breast cancers, and are the most critical diagnostic imaging tool we have to help detect breast cancer.
During a mammogram, your breast is placed on a plate by a trained technician and is pressed by another plate from above before taking a X-ray image. A typical screening mammogram will take two pictures of each breast. Mammograms should not be painful, but it sometimes helps to take a Tylenol or ibuprofen tablet 1 hour before your appointment to help minimize any discomfort.
Today, mammograms are performed with 3D / tomosynthesis technology, which helps your radiologist get an even better view of your breast tissue and minimize unnecessary further workup. This is actually even more comfortable than a traditional 2D mammogram, and is covered by insurance.
How often should women at high risk of developing breast cancer get a screening?
According to American Cancer Society, women with the following factors are categorized as women with high risk for developing breast cancer.
- Has a personal history of breast cancer.
- Has a first-degree family (parents, siblings and children) with a genetic mutation which increases risk of breast cancer, such as BRCA1 or BRCA2.
- Ashkenazi Jewish heritage
- Has a lifetime breast cancer risk greater than 20%
- Had chest radiation therapy between the ages of 10 and 30
It is also advised for a woman with high risk of developing breast cancer to discuss her screening option with her breast surgeon. High risk patients are usually recommended to undergo both breast MRI and mammogram screenings for early detection of breast cancer and for successful treatment.
See the American Society of Breast Surgeons Position Statement on Screening Mammography.
Breast cancer treatment
Breast cancer treatments are advancing all the time. People today have more options than ever before.
Your treatment plan will depend on the type of breast cancer, breast cancer stage and your overall health status. Even then, your treatment plan may vary vastly from another person with the same type and stage of breast cancer as you.
In cancer care, doctors specializing in different areas of cancer treatment—such as surgery, radiation oncology, and medical oncology—work together with radiologists and pathologists to create a patient’s overall treatment plan that combines different types of treatments. This type of cooperative team-based care is called multidisciplinary breast care, and is considered the gold standard for breast cancer treatment today.
Additionally, cancer care teams include a variety of other health care professionals, such as physician assistants, nurse practitioners, oncology nurses, social workers, pharmacists, counsellors, nutritionists, and others.
Factors affecting your treatment?
There is no single treatment course for breast cancer. Sometimes a tumor may be small but fast growing and other times a large tumor may be slow glowing. When it comes to breast cancer treatment, options and recommendations are personalized depending on several factors, such as:
- your type of breast cancer
- how advanced is your cancer, including how far it has spread outside of the breast
- tumor receptor status: estrogen, progesterone and HER2
- presence of hereditary genetic mutations such as BRCA1 and BRCA 2
Additionally, factors such as your age, other medical conditions and your personal preferences also play a major role in determining your breast cancer treatment plan.
DCIS and early-stage breast cancer
In both DCIS and early-stage breast cancer, your breast surgeon will discuss your options for surgery to remove the tumor. An important feature of breast cancer surgery is achieving negative margins around the tumor – this means making sure that the tumor is completely surrounded by healthy normal breast tissue before it is removed, to minimize leaving behind any cancer cells.
In addition to surgery, further radiation or chemotherapy may be recommended to prevent any microscopic cancer-causing cells to grow into a new tumor.
Large breast cancer tumors
In both large breast cancer tumors and tumors that are fast growing, doctors may recommend chemotherapy before performing surgery. The goal of this approach is to reduce the size of the tumor and thereby make it easier to remove the tumor through surgery. In fact, your breast surgeon may be able to perform a lumpectomy rather than a mastectomy if the tumor is significantly smaller.
Shared decision making
Your breast cancer treatment plan includes treatment for symptoms and side effects, which is an important part of cancer care. Take time to learn about all of your treatment options and be sure to ask questions about things that are unclear.
Talk with your doctor about the goals of each treatment and what you can expect while receiving the treatment. Shared decision making is particularly important for breast cancer because there are different treatment options. It is also important to check with your health insurance company before any treatment begins to make sure the treatment is covered.
Surgery for breast cancer
In breast cancer patients, surgery is performed to remove tumors. Surgery is also used to examine the nearby axillary lymph nodes, which are under the arms. These procedures are performed by surgical oncologists who specialize in treating breast cancer.
Depending on the type of your breast cancer and its staging two types of surgery are performed.
Lumpectomy / Partial Mastectomy
During lumpectomy, a small portion of your breast which contains the tumor is removed. Because you are able to keep your breast, this is called breast conserving surgery. The goal of lumpectomy is to remove tumor while maintaining the appearance of the breast.
Dr. Kolluri routinely uses the BioZorb device in combination with oncoplastic rearrangement to minimize the appearance of the lumpectomy site and decrease the defect associated with lumpectomy. In patients with significant breast ptosis (breast droopiness), a lumpectomy can be combined with a breast reduction or breast lift / mastopexy, performed by a plastic surgeon at the same time as lumpectomy. This is considered breast cancer reconstruction surgery, and is covered by insurance.
Mastectomy
Mastectomy is a surgical procedure to remove the entire breast mound. All mastectomies leave behind 2-5% of breast tissue.
Newer mastectomy techniques can preserve breast skin and allow for a more natural breast appearance following the procedure. This is also known as skin-sparing mastectomy. Additionally, certain patients may be a candidate to save the nipple skin, which is called a nipple-sparing mastectomy.
Surgery to restore shape to your breast — called breast reconstruction — may be done at the same time as your mastectomy or during a second operation at a later date.
There are many options for breast reconstruction including DIEP flap, latissimus flap and implant-based reconstruction.
Lymph node removal and analysis
When breast cancer travels in the body, typically the first place it will travel to is the lymph nodes that live in the underarm region. For this reason, it is important to assess whether those lymph nodes have cancer.
Patients with invasive breast cancer will have either a sentinel lymph node biopsy or an axillary lymph node dissection. If a patient has non-invasive breast cancer (DCIS), lymph node surgery may not be indicated.
Sentinel lymph node biopsy
Sentinel nodes are the first few lymph nodes into which cancer drains. Sentinel node biopsy is a surgical procedure to determine whether the primary breast cancer has spread to the lymph nodes as well. Prior to surgery, the breast will be injected with a tracer dye that helps your breast surgeon locate the sentinel lymph nodes during surgery. During the procedure, your surgeon typically identifies 1-3 sentinel nodes and and removes them. This can be done via a small incision in the underarm, or through the mastectomy incision.
If the nodes turn out to be free of any cancer, then your surgeon is unlikely to remove any more nodes. But if cancer is found in your lymph nodes then your surgeon may recommend removal of more lymph nodes and further chemotherapy treatment.
Axillary lymph node dissection
In an axillary lymph node dissection, the surgeon removes all of the lymph nodes from the underarm. Typically, this will be 20-30 lymph nodes.
The goal of this procedure is to check for cancer in lymph nodes of the armpit – how many nodes contain cancer and how much cancer has spread of them.
This procedure significantly increases the risk of lymphedema, which is chronic arm swelling due to lymphatic fluid accumulation. For this reason, lymphedema therapy with a certified therapist is critical to avoiding this complication of surgery and restoring function to the arm.
Breast reconstruction surgery
Women who have had a mastectomy or lumpectomy may want to consider breast reconstruction. You also can choose whether or not to reconstruct your nipple.
For patients having a lumpectomy, reconstruction may be done at the same time to improve the look of the breast and to make both breasts look similar.
For patients who have had a mastectomy, reconstruction surgery involves using either tissue taken from another part of the body or breast implants. Reconstruction is usually performed by a plastic surgeon. A person may be able to have reconstruction at the same time as the mastectomy or may have it at any time in the future.
Autologous or flap reconstruction surgery
This technique uses muscle and tissue from elsewhere in the body such as the back or belly or buttocks or upper thigh and moved to the chest to reshape the breast. During the procedure, blood vessels are cut and the surgeon attaches the moved tissue to new blood vessels in the chest. The gold standard of breast reconstruction is the DIEP flap, which uses skin, fat and blood vessels from the abdomen.
Because blood vessels are involved with flap procedures, these strategies are usually not recommended for a woman with a history of diabetes or connective tissue or vascular disease, or for a woman who smokes, as the risk of problems during and after surgery is much higher.
Talk with your doctor for more information about reconstruction options and a referral to a plastic surgeon. Remember to discuss the pros and cons of each procedure with your plastic surgeon and with women in your support group who have had similar procedures done.
Implant reconstruction
A breast implant uses saline-filled or silicone gel-filled forms to reshape the breast. Before having permanent implants, you may temporarily have a tissue expander placed that will create the correct sized pocket for the implant.
However, there can be problems with breast implants. Some women have problems with the shape or appearance. The implants can rupture or break, cause pain and scar tissue around the implant, or get infected. If subsequent radiation is needed, implants have a higher rate of wound breakdown and infection. Implants have also been rarely linked to other types of cancer.
Although these problems are very unusual, talk with your doctor about the risks. It is also advised to talk to women in your support group who have had breast reconstruction surgery with implants to have a better idea of what it feels like to have an implant.
Breast prosthesis
An external breast prosthesis is an artificial breast, which fits into a special mastectomy bra. It provides an option for women who plan to delay or not have reconstructive surgery. These can be made of silicone or soft material such as a Knitted Knocker. Breast prostheses can be made to provide a good fit and natural appearance for each woman.
Radiation treatment for breast cancer
Radiation therapy for breast cancer involves using high energy X-rays or other particles to kill breast cancer as cancer cells are susceptible to its effects than normal cells. This form of treatment usually involves quick weekday appointments in an outpatient radiation center for 3-6 weeks. External beam radiation is the most common type of radiation treatment and is given from a machine outside the body. This can be done for a full six-week course, but accelerated and partial breast radiation options are available for select breast cancer candidates which include a faster or lesser course of treatment.
Side effects of radiation therapy
Radiation therapy can cause side effects including fatigue, swelling of the breast, redness and/or skin discoloration and pain or burning in the skin where the radiation was directed, sometimes with blistering or peeling. Your doctor can recommend topical medication to apply to the skin to treat some of these side effects. Most patients recover fully without long term complications, and radiation is extremely well tolerated.
Chemotherapy for breast cancer
Chemotherapy for breast cancer uses drugs to target and destroy breast cancer cells usually by keeping the cancer cells from growing, dividing, and making more cells. These drugs are usually given intravenously through a needle or orally as a pill.
A chemotherapy regimen, or schedule, usually consists of a combination of drugs given in a specific number of cycles over a set period of time. The schedule varies depending on the drugs used. Doctors have found that giving the cycles of certain chemo drugs closer together can lower the chance of recurrence and improve survival for women with advanced inoperable breast cancer.
Chemotherapy for breast cancer frequently is used in addition to other treatments, such as surgery, radiation or hormone therapy. Receiving chemotherapy for breast cancer may increase the chance of a cure, decrease the risk of the cancer returning, alleviate symptoms from the cancer or help people with cancer live longer with a better quality of life.
If the cancer has recurred or spread, chemotherapy may control the breast cancer to help you live longer. Or it can help ease symptoms the cancer is causing.
Adjuvant chemotherapy
After you have surgery to remove a tumor, your doctor may recommend chemotherapy to kill any undetected cancer cells which, if left, may continue to form new tumors in the future.
Your doctor may recommend adjuvant chemotherapy if you have a high risk of the cancer recurring or spreading to other parts of your body, even if there is no evidence of cancer after surgery. You may be at higher risk of developing cancer in other parts of your body if cancer cells are found in lymph nodes near the breast with the tumor.
Neoadjuvant chemotherapy
Your doctor may recommend chemotherapy before surgery to shrink larger tumors. This may provide your surgical oncologist the best chance of removing the tumor completely. Neoadjuvant chemotherapy can also lead to a lumpectomy where a mastectomy would have otherwise been the only treatment option.
Neoadjuvant chemotherapy also enables evaluation of the tumor response to therapy, which helps clarify prognosis and the best chemotherapy drug choice.
Side effects of chemotherapy
The side effects of chemotherapy depend on the individual, the drugs used, whether the chemotherapy has been combined with other drugs, the schedule and dose used.
Side effects can include fatigue, risk of infection, nausea and vomiting, hair loss, loss of appetite, diarrhea, constipation, numbness and tingling, pain, early menopause, weight gain, and chemo-brain or cognitive dysfunction. These side effects can often be very successfully prevented or managed during treatment with supportive medications, and they usually go away after treatment is finished.
Rarely, long-term side effects may occur, such as heart damage, permanent nerve damage, or secondary cancers such as leukemia or lymphoma.
Hormone therapy for breast cancer
Hormonal therapy, also called endocrine therapy, is an effective treatment for those types of breast cancer with tumors that test positive for either estrogen or progesterone receptors.
This type of tumor uses hormones produced by the body naturally to fuel its growth. Blocking these hormones can help reduce the size of the existing tumor, prevent a cancer recurrence and death from breast cancer.
Hormonal therapy is used either by itself or after chemotherapy.
Neoadjuvant hormonal therapy is sometimes recommended before a breast surgery to remove tumor to shrink the tumor and enable the surgeon to do an effective operation, if chemotherapy cannot be given.
Adjuvant hormonal therapy can be recommended – sometimes for up to 10 years – to prevent the recurrence of cancer in patients with high-risk of developing breast cancer.
Hormonal therapy for premenopausal women
Ovaries produce estrogen and progesterone. These hormones not only govern the menstrual cycles in a premenopausal woman but they also help maintain a healthy skeletal system. But when these hormones fuel your type of breast cancer, then ovarian suppression or ovarian ablation may be recommended
Ovarian suppression and ovarian ablation
Ovarian suppression is the use of drugs to stop the ovaries from producing estrogen. Ovarian ablation is the use of surgery to remove the ovaries. These options may be used in addition to hormonal therapy.
For ovarian suppression, gonadotropin or luteinizing releasing hormone agonist drugs are used to stop the ovaries from making estrogen, causing temporary menopause. Since they are not very effective for treating breast cancer on their own, they are typically given in combination with other hormonal therapy.
For ovarian ablation, surgery to remove the ovaries is used to stop estrogen production. While this is permanent, it can be a good option for women who no longer want to become pregnant, especially since the cost is typically lower over the long term.
Hormonal therapy for women after menopause
Aromatase inhibitors are a class of medicines that reduce the amount of estrogen in your body, depriving breast cancer cells of the hormones they need to grow. Aromatase inhibitors are only used in women who have undergone menopause. They cannot be used unless your body is in natural menopause or in menopause induced by medications or removal of the ovaries.
Aromatase inhibitors are given as pills. Your doctor determines how long you continue aromatase inhibitors depending on your specific situation. Current research suggests that the standard approach would be to take these medications for up to 10 years, but every person is different and you and your doctor should carefully assess how long you should take them.
Targeted therapy for breast cancer
Targeted therapy for breast cancer is a treatment course that uses drugs to target specific genes and proteins that are the root cause for the growth and survival of cancer cells. For example, targeted therapy may block the action of an abnormal protein (such as HER2) that stimulates the growth of breast cancer cells.
Doctors often use targeted therapy along with chemotherapy and other treatments.
Monoclonal antibodies
Monoclonal antibodies are laboratory-manufactured proteins that bind with the certain cancer cancer cells and prevent them from growing and multiplying.
Monoclonal antibody drugs such as Herceptin target HER2-positive tumors. If cancer cells are positive for the HER2 receptors that means there is an overabundance of receptors on the cancer cell for the growth-stimulating HER2 protein.
The tumor acts almost like a magnet for growth hormones, and when the tumor cells connect with growth hormone cells, the cancer can quickly grow and multiply. Herceptin helps shrink these HER2-positive tumors by finding the cells, binding with them, and blocking the action of the receptor.
Side effects that most commonly occur during the first treatment include fever and chills. Other possible side effects include weakness, nausea, vomiting, diarrhea, headaches, difficulty breathing, and rashes.
These side effects generally reduce after the first treatment. Herceptin also may cause heart damage, heart failure, and serious breathing problems. Before and during treatment, your doctor will most likely check your heart and lungs.
Small-molecule drugs
Drugs called small-molecule drugs can block the process that helps cancer cells multiply and spread. Angiogenesis inhibitors are an example of this type of targeted therapy. Angiogenesis is the process for making new blood vessels. A tumor needs blood vessels to bring it nutrients. The nutrients help it grow and spread. Angiogenesis inhibitors starve the tumor by keeping new blood vessels from forming in the tissue around it.
Immunotherapy for breast cancer
Immunotherapy is designed to boost the body’s natural defenses to fight the cancer. It uses materials made either by the body or in a laboratory to improve, target, or restore immune system function.
Your immune system is designed to protect you from disease or infection causing bacteria, virus or fungus foreign. When these invaders enter your body, your immune system works to kill them. This self-defense system works to keep you from getting sick.
Immunotherapy uses substances either made naturally by your body or in laboratories to boost the immune system to stop, kill, spread or slow the growth of cancer cells.
To start an immune system response to a foreign invader, the immune system has to be able to tell the difference between cells or substances that are “self” (part of you) vs. “foreign” (not part of you and possibly harmful). Your body’s cells have proteins in them to help the immune system recognize them as “self.” This is part of the reason the immune system usually doesn’t attack your body’s own tissues.
“Foreign” cells have proteins and other substances on their surfaces and inside them that the body doesn’t recognize, called antigens. Foreign antigens trigger the immune system to attack them to either destroy them or keep them in check so they can’t harm the body.
There are two main reasons that stop your immune system from attacking breast cancer tumors.
A breast cancer cell starts out as a normal, healthy cell.
Cancer forms out of cells that were once normal and functional to the body. Early breast cancer cells don’t look any different from normal cells. They don’t produce antigens the way that bacteria, viruses, and other foreign materials do — which makes it challenging for the immune system to detect and attack them. But as cells transform into cancer, they do create proteins that the immune system sees as “foreign” antigens. In some cases, the immune system is able to recognize some cancer cells as harmful and stop the process before a cancer can grow further.
Cancer cells develop the ability to avoid the immune system.
Breast cancer doesn’t happen overnight; it develops over a period of time. As healthy cells gradually change into cancer cells, the genetic information inside them also changes. Some of these genetic changes allow the cancer cells to avoid detection by the immune system. Other changes allow cancer cells to speed up their growth rate and multiply much more quickly than normal cells do. This process can overwhelm the immune system and allow the breast cancer to grow unchecked.
Immunotherapy medicines can be divided into two main groups:
1. Active immunotherapy
Active immunotherapy is a treatment in which your immune system is stimulated to attack the cancer cells. Cells from a cancer are examined in the lab to find antigens specific to that tumor. Then an immunotherapy treatment is created that makes the immune system target those antigens. Cancer vaccines and adoptive cell therapy are examples of active immunotherapies.
2. Passive immunotherapy
Passive immunotherapy gives the body man-made immune system components to help it fight cancer. Passive immunotherapies don’t stimulate your immune system to actively respond the way active immunotherapies do. Immune checkpoint inhibitors and cytokines are examples of passive immunotherapies.
Because immunotherapy medicines help your immune system to kill cancer, the process can take a long time. Right now, it’s not clear how long someone should be treated with immunotherapy. Many experts believe that combining immunotherapies — for example, a vaccine with a checkpoint inhibitor — may be a good way to jump start a strong immune response to cancer. It’s also likely that immunotherapies will be combined with other cancer treatments, such as targeted therapies.
Newly Diagnosed with Breast Cancer
Breast cancer is not one disease. There are many types, stages and each case is different from the other.
When a person is diagnosed with breast cancer, information comes in overwhelmingly quickly. Even before the news sinks in, a swarm of physicians specializing in different fields follow with a plethora of information, all in new and sometimes scary vocabulary.
But the important thing to remember is that medical science and research for breast cancer treatment has advanced leaps and bounds. It is okay to get additional screening, imaging studies and opinions, and ask questions to understand the characteristics of your tumor and plan of care.
All breast cancers are not the same
Tumor size, presence of cancer cells in lymph nodes or other parts of the body and tumor biology are essential pieces of information about your specific breast cancer.
Your breast surgeon helps you understand three specific characters about your cancer and how it impacts your treatment options.
Stage
There are four stages to cancer, four being the most advanced. These stages describe the size of the tumor and the extent of which it has spread to other organs.
Hormone sensitive
When a tissue sample is collected, it is tested to see if it is sensitive to the hormones estrogen or progesterone. If your tumor is hormone receptor-positive, then hormone therapy may be recommended to suppress these hormones and thereby reduce the size of the tumor.
HER2
Your tissue sample will also be tested for sensitivity towards Human epidermal growth receptor (HER2), a protein that influences the growth and spread of cancerous tumors.
Factors that influence your breast cancer treatment plan
A clear understanding of the above information points you in the direction to research further towards your treatment options. There are three major factors that play a significant role in your cancer treatment plan.
Genetics
Some breast cancers are due to a mutation in genes such as BRCA1 and BRCA2. When these genes are mutated, or not working correctly, this can significantly increase the risk of breast cancer formation. This plays a significant role not only in your treatment plan but also future cancer screens for other types of cancers.
Fertility
Drug therapy (chemotherapy) and hormone therapy can affect fertility especially in women within the childbearing age. It is important to consult a fertility specialist prior to chemotherapy, and make an informed decision.
Once you have gathered all the information and have clarity of mind, together with your breast surgeon, you can then come with a multidisciplinary cancer care plan that is tailored for you.
Breast cancer treatment is a team effort
When you are diagnosed with breast cancer, it is important to know that you are not alone.
You have a team to help you navigate this diagnosis, and this team usually is made of a breast surgeon, medical oncologist and radiation oncologist (if radiation is necessary.) Other important members of the team can be a nurse navigator, physical therapist, genetic counselor, social worker, spiritual care provider, psychologist and therapist.
Additionally, depending on your specific case a dietitian, nutritionist and lifestyle counselor may be recommended.
Expect the first couple of weeks following your cancer diagnosis to be challenging. Your team, led by Dr. Kolluri, is here to support your goals of treatment and quality of life, to help provide you with the best survivorship experience possible.
Life After Breast Cancer
After going through a series of tests and treatment that might sometimes last upto a year, you may be eager for a taste of normalcy – for you to get back to your old life.
It is however important to remember that even though the treatment is over, your body and mind are still healing. Fatigue and other side effects like “chemo-brain” may not go away as soon as your treatment ends.
Be patient with yourself
Although you may be anxious to get back to school or work or home to take care of your family, you may notice that you have reduced cognitive ability and multi-tasking may seem like a challenge. Remember, whether it is surgery, radiation therapy, chemotherapy or hormone therapy, your body just went through a major trauma and needs time to recover.
Don’t hesitate to share your physical and mental condition with your family and friends. More often than most, they will only be understanding and support you further with your day-to-day activities.
The new normal
It might take over three months or more in some cases for your hair to grow back – and you may find your new hair has a lot more greys than they used to – for your skin and nails to feel healthy. But it might take longer for you to accept your new body. Standing in front of the mirror and taking a look at your body alone can be a traumatizing experience for many.
Yet for some the fear of relapse or fear that other members of your family might be diagnosed with breast cancer in future can be stressful too. Annual screenings after a successful treatment are usually anxiety inducing.
Talk to your medical team and if necessary, a therapist. These screening tests are meant to help diagnose a possible cancer in the very early stages, and it certainly does not mean that you will relapse for certain.
Share your story
Participate in support groups when you feel some of your energy returning and can confidently step out of the house. Sometimes knowing that there are others like you can bring immense hope. Sharing your story and journey towards surviving breast cancer may even help many who are fighting it and finding it hard to stay positive.
Embrace a healthier lifestyle
Equate surviving cancer to getting a second chance at life. Follow a healthy lifestyle – eat your greens, consume more vegetables, reduce oily and fatty foods that are high in carcinogens, reduce consumption of alcohol and other recreational drugs. If possible, quit smoking.
Exercise can also play a huge role in helping you feel energised. You need not have to train for a marathon, but a walk in the park or gentle yoga helps you feel both physically and mentally great.
Practice gratitude
Meditation and other mindful living habits help you deal with the entire ordeal and look at life with a positive outlook.
Life after breast cancer will certainly have its ups and downs. Some days will be easier and some hard. But you will have forever changed – you will notice that your perspective towards life is no longer the same and your priorities have changed. Some even try to live their lives to the fullest, follow their passions and try to not have any regrets.
QUICK LINKS
- What is breast cancer?
- Symptoms of breast cancer?
- Breast cancer diagnosis
- Breast cancer treatment
- Surgery for breast cancer
- Radiation treatment for breast cancer
- Chemotherapy for breast cancer
- Hormone therapy for breast cancer
- Targeted therapy for breast cancer
- Immunotherapy for breast cancer
- Newly diagnosed with breast cancer
- Life after breast cancer
